On this page:
Feature Highlights:
Evaluation of Bundled Care for Hip and Knee Replacements (2018 – 2020)
The evolution of Bundled Care and Integrated Funding continues in Ontario. Following the Integrated Funding Model demonstration project (see below), the Ministry of Health and Long-Term Care introduced Bundled Care for hip and knee replacements. The expansion included more than 20 healthcare teams that volunteered in 2018/19 and included all surgical centres as of April 2019. The Health System Performance Network was again involved in evaluating the expansion of bundled care. Our evaluation involved both qualitative and quantitative approaches. Qualitative interviews with key stakeholders were completed in two sites within each of 4 regions of the province ranging from urban Toronto to remote North West. These interviews focused on the implementation experiences, challenges and key success factors. Participants had many challenges and recommendations including burdens relating to administration and payment and greater attention to quality improvement. Our quantitative evaluation provides a time series analysis of key measures ranging from volumes and length of stay to readmissions, adverse events and rehabilitation care. Overall, integrating post-acute care within the bundled care payments did not substantially influence the trends in most measures except for increased outpatient and decreased inpatient rehabilitation volumes.

Central Evaluation of Integrated Funding Models (2015 – 2019)
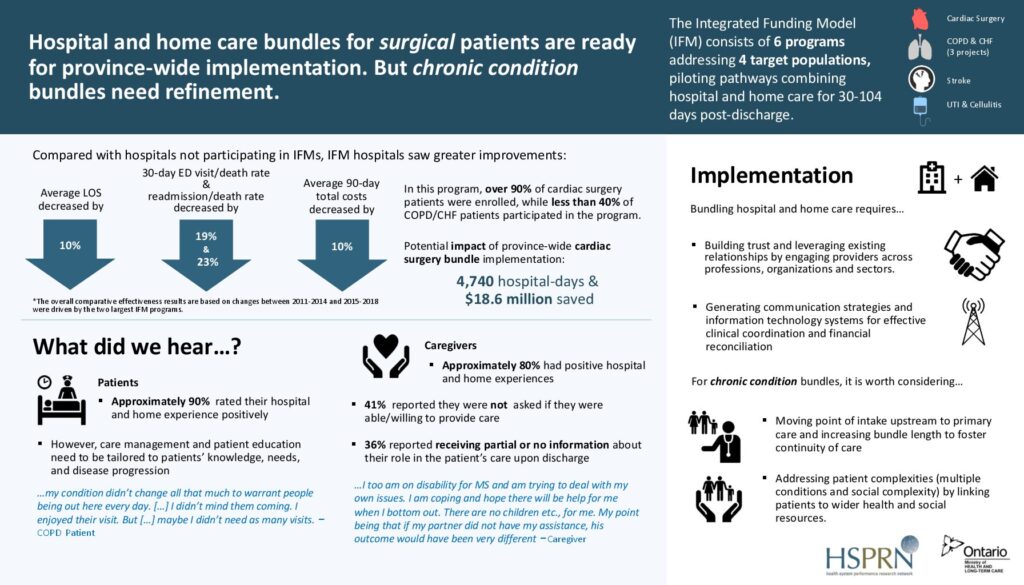
In 2015, the Ministry of Health and Long-Term Care (MOHLTC) called for proposals to participate in an Integrated Funding Model (IFM) initiative. Six projects were selected to test innovative approaches to integrate care and funding over a patient’s episode of care. The episode of care began in acute care and included a transition to community-based post-acute care. The goal of the IFM was to improve efficiency and value for money as well as patient, caregiver and provider experience.
The work undertaken by the HSPN has identified local barriers to integrating funding and successful processes for IFMs throughout the province. Evidence has been reviewed by senior management and policymakers, as well as service delivery partners, and has played a crucial role in decisions made to spread of IFMs and bundled care throughout Ontario.

Information
The evaluation aimed to:
- Identify success factors and potential barriers to implementation.
- Measure patients’ health outcomes.
- Measure and report healthcare resource utilization, costs, as well as patient, caregiver, and provider experiences.
- Inform policy and guide potential provincial spread.
The central evaluation of 6 selected IFM programs used a mixed-method design and consisted of four components:
- Qualitative interviews for implementation insights.
- Quantitative surveys and qualitative interviews for patient and caregiver experiences.
- Ongoing monitoring and reporting of common indicators.
- Comparative effectiveness analysis.
Despite varying patient populations and provider groups, common early success factors emerged, including partnerships, trust, leadership, and operational cohesiveness. Challenges such as sharing clinical information, financial pressures, and competing priorities were prevalent. Patients generally reported positive experiences in hospital and home care, with notable challenges during the transition from acute to home care. Caregivers often lacked awareness of patient needs and involvement opportunities. The IFM program showed significant decreases in key metrics across all patients compared to non-IFM hospitals, with the two largest programs demonstrating independent significance. Programs focused on chronic conditions like COPD/CHF faced enrolment challenges but showcased potential improvements, suggesting enhancements in health resources, such as physician compensation, making the program more patient-centred and responsive to individual needs.
Overall the IFM program was associated with positive patient outcomes and reduced healthcare costs. Much of the overall success of the IFM initiative is attributable to the two largest projects (MH-PPATH and HNHB ICC 2.0). If both initiatives were rolled out provincially with the same uptake and success, an estimated annual savings of $42.7M could be realized. The bundled approach to care was a valuable strategy to pursue. It appeared to be easier to implement bundled care for short-term and generally more predictable surgical care pathways. We recommend expanding bundled care quickly to all surgical care and to further exploring the improvements that are needed for the model to be successful for all patients who require ongoing care for chronic medical conditions.
Research Methods
Implementation Evaluation
Patient and Caregiver Experience
Baseline (2014) and Quarterly (2015-2018)
Comparative Effectiveness Analysis
Recent IFM Publications
Central Evaluations of Integrated Funding Models
2019
Hospital and Home Care Bundles for Surgical Patients Are Ready for Province-Wide Implementation. but Chronic Condition Bundles Need Refinement.
2019
Integrated Funding Models Central Evaluation
2019